Top Surgery Journal Articles
2024
Mastectomy Surgical Recommendations for Female-to-Male Transgender Patients, and a Discussion of Gender-Affirming Care for Gender-Dysphoric Adolescents.
Gupta A, Marvel J. The American Journal of Cosmetic Surgery. 2024;0(0).
By consistently using the technique described in this article, surgeons can achieve consistent and aesthetically pleasing Top Surgery results. Multiple states in the United States are seeking to ban this type of care and are even attempting to restrict health care for adults. These bans are being enacted despite carefully researched and written guidelines from major international organizations. By following these guidelines, physicians can provide safe and evidence-based care to adolescents.
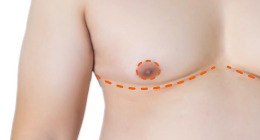
Patient-Reported Outcomes on Subjective Nipple Sensation After Double-Incision and Periareolar Mastectomy for Chest Masculinization: Subjective Nipple Sensation After Chest Masculinization.
Chen A, Garvey SR, Nanda AD, Friedman R, Jia E, Morgenstern M, Barron S, Tobias A, Cauley RP. Ann Plast Surg., 2024 Apr 1;92(4):383-388.
We found that nipple sensation may be associated with postoperative nipple satisfaction. Operative techniques to optimize nipple sensation preservation may improve this population's postoperative satisfaction.
2021
Low Risk of Persistent Pain, Sensory Disturbances, and Complications Following Mastectomy After Gender-Affirming Surgery. [FULL TEXT]
Lang CL, Day DL, Klit A, Mejdahl MK, Holmgaard R. Transgend Health. 2021 Jul 30;6(4):188-193.
There is currently no literature on postsurgical pain in trans men after mastectomy. We aimed at investigating the prevalence and severity of postsurgical persistent pain, sensory disturbances, and complications in trans men after mastectomy. Although a quarter of the patients in the study experienced persistent pain the pain is mild, not constant, and can be treated with weak analgesics. Trans men undergoing mastectomy should be thoroughly informed about this complication before surgery.
Chest
Masculinization Technique and Outcomes in 72 Double-incision
Chest-contouring Procedures with Free Nipple Grafting. [FULL
TEXT]
Alexandra I. Naides, BFA, Jerette J. Schultz, MD, Nikita O.
Shulzhenko, MD, and Jonathan D. Keith, MD, FACS. Plast
Reconstr Surg Glob Open. 2021 Mar; 9(3): e3459.
The authors present the outcomes of 72 consecutive chest
masculinization cases using the double-incision technique with
free nipple grafting.
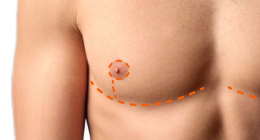
Classification of Transgender Man's Breast for
Optimizing Chest Masculinizing Gender-affirming Surgery [FULL
TEXT]
Wolf, Yoram MD, Kwartin, Samuel MD. Plastic and
Reconstructive Surgery. Jan 2021, Vol 9, Issue 1.
A number of algorithms have been proposed for selecting the
surgical technique; these have generally been based on the degree
of breast ptosis and the quality and elasticity of the skin. We
present a series of subcutaneous mastectomies operated on by 1
surgeon during the last 2 decades. Based on our experience, we
suggest a classification system for selecting surgical technique.
Recognizing the Importance of Chest Surgery for
Transmasculine Youth
Laura E. Kuper, G. Nic Rider and Colt M. St. Amand. Pediatrics,
February 2021.
Transmasculine youth and adults often report that masculinizing
chest surgery (MCS) is an important step toward gender
affirmation. However, most research in this area has been focused
on adults. In this issue of Pediatrics, Mehringer et al elicit
transmasculine youth's descriptions of their experiences with
chest dysphoria and MCS. Youth described improvements in mental
health and quality of life after MCS. Although barriers to
gender-affirming care remain widespread for transgender adults,
barriers are particularly pronounced for youth. As youth in this
study describe, lack of access to MCS prolongs unnecessary
distress and difficulties in functioning.
2020
Surgical and patient-reported outcomes following
double incision and free nipple grafting for female to male
gender affirmation: does obesity make a difference?
Michael J. Stein, Emma Grigor, Jacob Hardy, Mario Jarmuske. Journal
of Plastic, Reconstructive & Aesthetic Surgery,
December 10, 2020.
Chest wall contouring using the Double Incision technique
continues to be safe and effective for the management of gender
dysphoria in transmale and nonbinary patients. Considering that
obese patients have comparable surgical and patient-reported
outcomes as non-obese patients, it is our practice to routinely
offer the DIFNG technique to healthy obese patients with BMI's
between 30 and 40.
A Three-Step Technique for Optimal Nipple
Position in Transgender Chest Masculinization
Haripriya S Ayyala, MD, Thayer J Mukherjee, MD, Thuy-My Le, MSE,
Wess A Cohen, MD, Margaret Luthringer, MD, Jonathan
D Keith, MD, FACS. Aesthetic Surgery Journal,
Volume 40, Issue 11, November 2020, Pages NP619–NP625.
The ideal position of the nipple-areola complex (NAC) in the
transgender population can be a challenge to determine. The triple
confirmation technique is an easy, reproducible method to guide
the surgeon in relocation of the NAC.
Double
Incision Mastectomy with Free Nipple Graft for Masculinizing
Chest Wall Surgery [FULL TEXT]
Shervin A. Etemad, MD, William M. Furuyama, BS, and Julian S.
Winocour, MD. Plast Reconstr Surg Glob Open. 2020 Nov;
8(11): e3184.
Although the literature about top surgery continues to document
advances in technique and aesthetic outcomes, there is still
significant room for improvement in the development of
patient-centered outcomes. Given the increasing number of
gender-affirming operations in the United States and the
increasing evidence indicative of significant positive change,
continued improvement and understanding of top surgery and other
gender-affirming surgeries are essential.
Crowdsourcing
the Ideal Nipple-Areolar Complex Position for Chest
Masculinization Surgery. [FULL TEXT]
Cohen, W. A., Maisner, R. S., Hazim, N., Ayyala, H. S., & Keith, J. D.
(2020). Plastic and reconstructive surgery. Global open,
8(8), e3070.
Chest masculinization surgery is increasing in prevalence.
However, the ideal location of the nipple-areolar complex (NAC) is
unknown. Our purpose was to determine the most aesthetically
favorable male NAC position for use in chest masculinization
through crowdsourcing. Ultimately, NAC localization during chest
masculinization will be the result of shared decision-making
between the patient and the surgeon to fulfill each patient’s
aesthetic goals.
Free Nipple Grafts: What to Expect During the
Healing Process
Alvina Won MD, E. Antonio
Mangubat, MD. The American Journal of Cosmetic Surgery,
Vol. 37, Issue 4, April 26 2020.
There is little documentation available that clearly describes the
healing process of free nipple grafts for patients and their
caregivers. The nipple-areolar complex is harvested as a
full-thickness skin graft. It is resized and repositioned to
conform to a more masculine aesthetic. A bolster of nonadherent
dressing is tied over the graft and left in position for 7 days as
adherence, imbibition, and inosculation occur. The superficial
layer of epidermis of the graft initially exfoliates as it is
replaced by upwardly migrating cells of follicular epithelium.
This is observed as a sloughing which can be disturbing to the
patient although it is an expected progression of the healing
process. Viable pink dermis will be seen underneath. Pigmentation
of the nipple graft can take 3-9 months.
A
Comparison of Gender-Affirming Chest Surgery in Nonbinary Versus
Transmasculine Patients.
McTernan M, Yokoo K, Tong W. Ann Plast Surg. 2020 Feb 6.
Increasingly more nonbinary patients are obtaining better access
for gender-affirming chest surgery (top surgery), representing an
important subset of patients who undergo such surgery. There were
111 nonbinary patients and 665 transmasculine patients included in
the final analyses.
Analysis of Chest Masculinization Surgery Results
in Female-to-Male Transgender Patients: Demonstrating High
Satisfaction beyond Aesthetic Outcomes Using Advanced Linguistic
Analyzer Technology and Social Media [FULL TEXT]
Black, Cara K.; Fan, Kenneth L.; Economides, James M.; Camden,
Rachel C.; Del
Corral, Gabriel A. Plastic and Reconstructive Surgery,
Jan 2020 - Volume 8 - Issue 1 - p e2356.
Despite wide variety in surgical appearance, there is a high level
of satisfaction and community support. This is in contrast to the
low-quality ratings by plastic surgeons. The results demonstrate
the strong psychological and functional underpinnings chest
masculinization has for patients. However, surgical results can be
improved through a variety of techniques such that patients have
both excellent surgical results and high satisfaction.
Are
Prophylactic Postoperative Antibiotics Necessary after
Masculinizing Mastectomy with Free Nipple Graft? A
Single-institution Retrospective Review
Oren Ganor, Nicholas G Cuccolo, Divya Jolly, Elizabeth R Boskey.
Plast Reconstr Surg Glob Open, 2020 Jan 27;8(1):e2615.
Antibiotic overuse, particularly in the postoperative period, has
contributed substantially to increased rates of antibiotic
resistance. The aim of this case series was to report
postoperative outcomes following chest masculinization with free
nipple grafts performed according to a strict antibiotic protocol,
which restricted prophylaxis to a single preoperative dose, in the
absence of specific risk factors indicating a need for
postoperative antibiotics. In this case series featuring 62
consecutive patients undergoing chest reconstruction with 124 free
nipple grafts, there were no nipple losses or nipple graft
infection events.
2019
Continued
Barriers to Top Surgery among Transgender Men.
Nolan I, Poudrier G, Motosko C, Cook T, Saia W, Gothard M, Hazen
A. Plast Reconstr Surg. 2019 Dec 2.
This survey examined barriers to transition-related care via a
survey of insured transgender men and nonbinary individuals who
underwent masculinizing top surgery.
Female-to-Male Transgender Chest Contouring - A
Systematic Review of Outcomes and Knowledge Gaps
Cohen, Wess A. MD; Shah, Nikhil R. BA; Iwanicki, Margaret MD;
Therattil, Paul J. MD;
Keith, Jonathan D. MD, FACS. Annals of Plastic Surgery:
November 2019 - Volume 83 - Issue 5 - p 589-593.
As the surgical treatment of gender dysphoria continues to grow,
it is imperative for plastic surgeons to understand the surgical
options and associated outcomes for transmasculine top surgery.
Future research is needed to improve patient selection, surgical
decision making, and patient-reported outcomes for different chest
contouring techniques. In addition, there is a significant
knowledge gap for the ideal nipple-areolar complex shape, size,
and location.
Mastectomy
in Transgender and Cisgender Patients: A Comparative Analysis of
Epidemiology and Postoperative Outcomes.
Cuccolo N, Kang C, Boskey E, Ibrahim A, Blankensteijn L, Taghinia
A, Lee B, Lin S, Ganor O. Plast Reconstr Surg,2019 Jun
12;7(6):e2316.
The aim of this study was to provide a nationwide assessment of
epidemiology and postoperative outcomes following masculinizing
mastectomy and compare them with outcomes following mastectomy for
cancer prophylaxis and gynecomastia correction in cisgender
patients. Mastectomy is a safe and efficacious procedure for
treating gender dysphoria in the transgender male, with an
acceptable and reassuring complication profile similar to that
seen in cisgender patients who approximate either the natal sex
characteristics or the new hormonal environment.
What
is "Nonbinary" and What Do I Need to Know? A Primer for Surgeons
Providing Chest Surgery for Transgender Patients.
Esmonde N, Heston A, Jedrzejewski B, Ramly E, Annen A, Guerriero
J, Hansen J, Berli
J. Aesthet Surg J. 2019 Apr 8;39(5):NP106-NP112.
This was an observational study of nonbinary patients who
underwent "chest-affirming surgery" from 2012 to 2017. A total of
458 patients with gender dysphoria underwent chest surgery; 58
(13%) patients were nonbinary. The most commonly performed
procedure was the double incision technique with nipple grafts
(72%). Chest surgery for nonbinary patients comprises a
considerable proportion of transgender surgery practice, and
surgeons who provide affirming care should be familiar with the
unique characteristics and treatment options for this population.
Nipple areolar complex reconstruction is an
integral component of chest reconstruction in the treatment of
transgender and gender diverse people.
International Journal of Transgenderism, 20:1, 1-3, 2019.
There has been a growing trend for insurance companies in the
United States to deny coverage of nipple areolar reconstruction
for transgender patients undergoing chest masculinization. We, the
undersigned, representing the national leaders in gender affirming
surgical treatment are writing to state our joint and expert
opinion that nipple and areolar reconstruction in trans masculine
chest surgery is an inherent and irrefutable part of treatment for
transgender and gender diverse individuals undergoing mastectomy
for gender dysphoria. We cite our concerns regarding insurance
denials for this medically necessary procedure.
Assessing
Quality of Life and Patient-Reported Satisfaction with
Masculinizing Top Surgery: A Mixed-Methods Descriptive Survey
Study.
Poudrier G, Nolan I, Cook T, Saia W, Motosko C, Stranix J, Thomson
J, Gothard M, Hazen A. Plast Reconstr Surg. 2019
Jan;143(1):272-279.
Following top surgery, measures of quality of life and sexual
confidence improved significantly. In addition, 86 percent
reported improvement in gender dysphoria-related mental health
conditions. All but one respondent reported that top surgery had
an overall positive impact on their life. Top surgery had major
positive effects on all mental health and quality-of-life metrics.
The authors' findings contribute to a much-needed body of evidence
that top surgery markedly improves the daily lives and functioning
of transgender and nonbinary individuals who choose to undergo it.
Female-to-Male
Gender-Affirming Chest Reconstruction Surgery.
Ammari T, Sluiter E, Gast
K, Kuzon WM Jr. Aesthet Surg J. 2019 Jan 17;39(2):150-163.
An appraisal of the available literature on top surgery to allow
plastic surgeons to understand current practices and determine the
best surgical technique using a decision algorithm and the
patient's preoperative anatomy and characteristics.
2018
A
Single Surgeon's Experience With Transgender Female-to-Male
Chest Surgery.
Whitehead D, Weiss PR, Podolsky D. Ann Plast Surg. 2018
Sep;81(3):353-359.
Any of the reviewed techniques are safe in practice; however,
there is a learning curve associated with their use, and longer
follow-up will allow for the identification of late complications.
The double incision with nipple transposition on a pedicle
technique can be considered for patients for whom depigmentation
of the nipple-areola complex is a significant concern, especially
if they are willing to tolerate a potentially suboptimal chest
contour.
Modified
Nipple Flap with Free Areolar Graft for Component Nipple-Areola
Complex Construction: Outcomes with a Novel Technique for Chest
Wall Reconstruction in Transgender Men.
Frey J, Yu J, Poudrier G, Motosko C, Saia W, Wilson S, Hazen A. Plast
Reconstr Surg. 2018 Aug;142(2):331-336.
The senior author's (A.H.) technique for component nipple-areola
complex creation in chest wall reconstruction for trans men with a
modified skate flap and free areolar graft, in conjunction with
double-incision mastectomy, is described. The use of a modified
nipple flap and free areola graft in transgender chest wall
reconstruction for trans men allows for flexible, component
construction of the male nipple-areola complex in a safe and
effective manner.
Chest
Surgery for Transgender and Gender Nonconforming Individuals.
Claes K, D'Arpa S, Monstrey SJ. Clin Plast Surg. 2018
Jul;45(3):369-380.
Chest surgery can greatly facilitate the experience of living in a
gender role. Transmasculine chest surgery includes mastectomy and
creation of a male chest. Preoperative parameters to be evaluated
include breast volume, degree of excess skin, nipple-areola
complex size and position, and skin elasticity.
Masculinizing
Top Surgery: A Systematic Review of Techniques and Outcomes.
Wilson SC, Morrison SD, Anzai L, Massie JP, Poudrier G, Motosko
CC, Hazen A. Ann Plast Surg. 2018 Feb 2.
Limited data exist comparing commonly used techniques in
masculinizing top surgery, and most are single institution
studies. A systematic review was performed on primary literature
dedicated specifically to the technical aspects and outcomes of
mastectomy for masculinizing top surgery. For each study, patient
demographics and surgical outcomes were compared. This analysis
notes several significant differences with regard to percentage
requiring acute reoperation and percentage requiring secondary
revision based on technique. Candidates for masculinizing top
surgery should be educated on these differences.
Female-to-Male Gender Affirming Top Surgery: A
Single Surgeon's 15-Year Retrospective Review and Treatment
Algorithm
Giancarlo McEvenue, Fang Zhou Xu, Runting Cai, Hugh McLean.
Aesthetic Surgery Journal, Volume 38, Issue 1, January 2018, Pages
49–57.
Of the 679 patients, 15.3% underwent Keyhole and the remaining
84.7% underwent DIFNG procedure. The total complication rate was
18.1% and the total reoperation rate was 11.2% and these rates
were shown to decrease over time. The two techniques differed
significantly (P < 0.001) in operating time (136 vs 102 min),
breast weight excised (215 vs 638 g), and complication rate (33 vs
16%). The aesthetic rating of results was 4.6/5 for Keyhole and
3.7/5 for DIFNG. Safe and aesthetically pleasing results were
achieved using this simplified algorithm. Experience with FTM
techniques can decrease complication and reoperation rates over
time.
2017
Creation
of an Aesthetic Male Nipple Areolar Complex in Female-to-Male
Transgender Chest Reconstruction.
Agarwal C, Wall V, Mehta S, Donato D, Walzer N. Aesthetic
Plast Surg. 2017 Dec;41(6):1305-1310.
Llittle detail is written on methods for creating a male appearing
nipple areolar complex (NAC) from a female NAC utilizing free
nipple graft techniques. Incorrect positioning of the NAC on the
chest wall and suboptimal shaping and sizing of the NAC are common
pitfalls in male NAC creation. Our anatomic study supports
placement of the male NAC relative to lateral and inferior borders
of the pectoralis muscle. Nipple grafting techniques presented
allow for a simple and reproducible method of creating an
aesthetic male NAC shape in female-to-male transgender chest
reconstruction.
Female-to-Male
Chest Reconstruction: A Review of Technique and Outcomes.
Donato DP, Walzer NK, Rivera A, Wright L, Agarwal CA. Ann
Plast Surg. 2017 Sep;79(3):259-263.
Critical evaluation of techniques, complications, and outcomes is
important particularly as the surgery becomes more commonly
performed. A retrospective review was performed of all patients
undergoing female-to-male chest wall reconstruction from 2008 to
2015. Charts were reviewed to evaluate patient demographics,
intraoperative details, and postoperative outcomes. Complications
were stratified into major and minor complications based on the
need to return to the operating room. Inframammary fold techniques
and periareolar techniques cohorts were compared for major
complications, minor complications, and need for revision
surgeries. Our patient cohort demonstrates that female-to-male
patients who undergo chest wall contouring through a transverse
inframammary fold incision with either composite or standard free
nipple grafting have decreased rates of revision surgery and trend
toward having lower complication rates as compared with
periareolar and limited scar techniques. To best manage
expectations, patients undergoing a periareolar or other limited
incision technique are counseled regarding an increased risk of
hematoma and an increased likelihood of revisions.
Surgical
Indications and Outcomes of Mastectomy in Transmen: A
Prospective Study of Technical and Self-Reported Measures.
[FULL TEXT]
van de Grift TC, Elfering L, Bouman MB, Buncamper ME, Mullender
MG. Plast Reconstr Surg. 2017 Sep;140(3):415e-424e.
The objectives of the present study were to prospectively follow a
cohort of transmen undergoing mastectomy to assess technical and
self-reported outcomes and to evaluate surgical decision-making.
Fifty-four transmen were recruited during a 10-month period at the
Department of Plastic Surgery of the Centre of Expertise on Gender
Dysphoria. Preoperative assessment included standardized chest
examination. Six months postoperatively, participants rated their
satisfaction with surgery, and 12-month postoperative surgical
outcomes were reviewed independently. Compared with inframammary
skin resections, concentric circular mastectomy-despite being
performed in favorable breast types-appears to produce poorer
technical and self-reported outcomes.
Aesthetic Female-to-Male Chest Transformation:
Power of Combining Modified Mastectomy with a Pectoral Implant
[FULL TEXT]
Abbed, Turkia; Shifrin, David A. Plastic and Reconstructive
Surgery, August 2017 - Volume 5 - Issue 8 - p e1445.
The technique for female-to-male "top" surgery combining
traditional mastectomy techniques with a complete lower pole
pedicle vascularized nipple-areola complex (NAC) and a pectoral
implant to shape the ideal male aesthetic chest.
A
Review of 101 Consecutive Subcutaneous Mastectomies and Male
Chest Contouring Using the Concentric Circular and Free Nipple
Graft Techniques in Female-to-Male Transgender Patients.
Knox ADC, Ho AL, Leung L, Hynes S, Tashakkor AY, Park YS, Macadam
SA, Bowman CC. (Vancouver, British Columbia, Canada; and Chicago,
Ill.) Plast Reconstr Surg. 2017 Jun;139(6):1260e-1272e.
One hundred one consecutive female-to-male transgender patients
undergoing subcutaneous mastectomy using the concentric circular
or free nipple graft technique were retrospectively reviewed. In
patients who meet selection criteria, the concentric circular
technique is preferred because of fewer scars, improved aesthetic
contour, and potential for retained nipple sensation. These
patients must be counseled regarding the higher rate of
complications and revisions. It was determined that smokers and
those with a nipple-to-inframammary fold distance greater than 7
cm or nipple-to-inframammary fold distance less than 7 cm and a
body mass index greater than 27 kg/m should undergo the free
nipple graft technique because of the increased risk of
complications with the concentric circular technique.
Masculine
Chest-Wall Contouring in FtM Transgender: a Personal Approach.
Lo Russo G, Tanini S, Innocenti M. (Department Plastic and
Reconstructive Microsurgery, Careggi Universital Hospital,
Florence, Italy) Aesthetic Plast Surg. 2017
Apr;41(2):369-374.
Between July 2013 and June 2016, 25 FtM transgender patients
underwent surgical procedures to create a masculine chest-wall
contour. In our study, we just considered 16 patients who have
undergone chest surgery with the double incision method. The
patients' survey revealed a high satisfaction rate with the
aesthetic result. In our group, no complications occurred, and two
patients have undergone supplementary surgery for axillary dog-ear
revision and nipple reconstruction. The authors propose a new
technical approach and indications for FtM transgender patients'
surgery. A longer scar that emphasizes the pectoralis muscle, a
smaller nipple and a resized and refaced areola are the key points
of our technique to give a masculine appearance to the chest. The
scars are permanent, but most of them will fade and the patients
are enthusiastic with their new "male" chest appearance. The high
level of satisfaction, the great aesthetic result and the low rate
of complications suggest to us the use of this technique in
medium- and large-size breasts.
Transsexual
Mastectomy: Selection of Appropriate Technique According to
Breast Characteristics
Hüsamettin Top and Serkan Balta. Balkan Med J. 2017 Mar; 34(2):
147–155.
The main objective of subcutaneous mastectomy is to create an
aesthetically pleasing male chest contour by removing all
glandular tissue while minimizing chest wall scars. The authors
recommend their point of view to aid in selecting the most
suitable subcutaneous mastectomy technique depending on breast
characteristics.
Chest-wall contouring surgery in female-to-male
transgender patients: A one-center retrospective analysis of
applied surgical techniques and results. [FULL TEXT]
Kääriäinen M, Salonen K, Helminen M, Karhunen-Enckell U. Scand
J Surg. 2017 Mar;106(1):74-79.
Female-to-male transgender patients undergoing chest-wall
contouring surgery at Tampere University Hospital between January
2003 and April 2015 were enrolled in the study. Breast appearance
was evaluated and either a concentric circular approach or a
transverse incision technique was used for mastectomy. The larger
the breast, poorer the skin quality, and greater the amount of
excess skin, the longer the required incision and resulting scar
is for mastectomy of female-to-male patients. Hematoma is the most
common reason for acute reoperation and secondary corrections are
often needed.
Top Surgery in Transgender Men: How Far Can You
Push the Envelope?
Bluebond-Langner,
Rachel; Berli,
Jens U.; Sabino, Jennifer; Chopra, Karan; Singh, Devinder;
Fischer, Beverly. Plastic & Reconstructive Surgery:
April 2017 - Volume 139 - Issue 4 - p 873e–882e.
The authors present their grading scale and the outcomes of the
largest cohort of top surgery published to date. Application of
this grading system can help determine which patients will benefit
from a subcutaneous mastectomy with free nipple graft versus a
circumareolar technique, with the primary endpoint being need for
aesthetic revisions.
2016
Body Image in Transmen: Multidimensional
Measurement and the Effects of Mastectomy [FULL TEXT]
Tim C. van de Grift, Baudewijntje P.C. Kreukels, Lian Elfering,
Müjde Özer, Mark-Bram Bouman, Marlon E. Buncamper, Jan Maerten
Smit, Margriet G. Mullender. The Journal of Sexual Medicine
Volume 13, Issue 11, November 2016, Pages 1778-1786.
Top Surgery positively influences body image more broadly than
satisfaction with the chest alone. Positive evaluation of the body
and decreased dysphoria during social situations were associated
with increased quality of life and self-esteem. Despite this
positive effect, there appears to be some residual body image
issues at this point of follow-up.
Health
impact of chest binding among transgender adults: a
community-engaged, cross-sectional study.
Sarah Peitzmeier, Ivy Gardner, Jamie Weinand, Alexandra Corbet,
Kimberlynn Acevedo. Culture, Health & Sexuality, May 2016.
Chest binding involves the compression of chest tissue for
masculine gender expression among people assigned a female sex at
birth, particularly transgender and gender non-conforming
individuals. There are no peer-reviewed studies that directly
assess the health impacts of chest binding, yet transgender
community resources commonly discuss symptoms such as pain and
scarring. A cross-sectional 32-item survey was administered online
to an anonymous, non-random sample of adults who were assigned a
female sex at birth and had had experience of binding (n = 1800).
Multivariate regression models were used to identify practices
associated with self-reported health outcomes. Of participants,
51.5% reported daily binding. Over 97% reported at least one of 28
negative outcomes attributed to binding. Frequency (days/week) was
consistently associated with negative outcomes (22/28 outcomes).
Compression methods associated with symptoms were commercial
binders (20/28), elastic bandages (14/28) and duct tape or plastic
wrap (13/28). Larger chest size was primarily associated with
dermatological problems. Binding is a frequent activity for many
transmasculine individuals, despite associated symptoms. Study
findings offer evidence of how binding practices may enhance or
reduce risk. Clinicians caring for transmasculine patients should
assess binding practices and help patients manage risk.
2015 and Earlier
Sexual
reassignment surgery in female-to-male transsexuals: an
algorithm for subcutaneous mastectomy.
Wolter A, Diedrichson J, Scholz T, Arens-Landwehr A, Liebau J. J
Plast Reconstr Aesthet Surg. 2015 Feb;68(2):184-91. doi:
10.1016/j.bjps.2014.10.016.
In this study, we introduce an algorithm to facilitate choosing
the appropriate mastectomy technique depending on morphological
aspects.
Improved
results after implementation of the Ghent algorithm for
subcutaneous mastectomy in female-to-male transsexuals.
Bjerrome Ahlin H, Kölby L, Elander A, Selvaggi G.
J Plast Surg Hand Surg. 2014 Dec;48(6):362-7. doi:
10.3109/2000656X.2014.893887. Epub 2014 Mar 11.
At the Sahlgrenska University Hospital, a two-step procedure was
used for mastectomies through 2002-2011. With this procedure, all
patients were operated on with a concentric circular incision in
the first session of surgery, followed by a second session 7-12
months later. From July 2011, a new approach was adopted, which
consists of treating patients according to the algorithm and
methods described by Monstrey et al. The aim of this study is to
evaluate these two different approaches and determine if similar
results, possibly with fewer surgeries and overall lower
complication rate, can be achieved by using multiple techniques
and a decision-making algorithm as compared to the two-step
approach where only a concentric circular technique was used.
Effects of Testosterone Treatment and Chest
Reconstruction Surgery on Mental Health and Sexuality in
Female-To-Male Transgender People
Samuel A. Davis & S. Colton Meier, Pages 113-128, Aug 2013.
Results indicate that testosterone treatment in FTMs is associated
with a positive effect on mental health on measures of depression,
anxiety, and anger, while Chest Reconstruction Surgery appears to
be more important for the alleviation of body dissatisfaction. The
findings have particular relevance for counselors and health care
providers serving FTM and gender-variant people considering
medical gender transition.
The
case for bilateral mastectomy and male chest contouring for the
female-to-male transsexual [FULL TEXT]
C Richards and J Barr. Ann R Coll Surg Engl. 2013 Mar;
95(2): 93–95.
The literature showed that Top Surgery is necessary for trans men
to live safely and effectively in their reassigned gender role,
and further that it acts as a prophylaxis against distress,
ameliorates extant distress as well as providing improved quality
of life and global functioning for this patient group.
Subcutaneous
mastectomy in female-to-male transsexuals: a retrospective
cohort-analysis of 202 patients.
Cregten-Escobar P, Bouman MB, Buncamper ME, Mullender MG. J
Sex Med. 2012 Dec;9(12):3148-53.
This study shows a correlation between the surgical technique,
complication rate, and length of hospital stay. The largest series
of subcutaneous mastectomies in female-to-male transsexuals to
date is presented. In general, the larger the breast, the larger
the scars that remain after the operation. On the other hand, the
smaller the scars resulting from the operation, the higher the
risk of hematoma.
Operative
management and techniques of mastectomy in female-to-male
transsexuals.
Morath S, Papadopulos N, Schaff J. Handchir Mikrochir Plast Chir.
2011 Aug;43(4):232-9. doi: 10.1055/s-0031-1273735. Epub 2011 May
17.
All procedures were conducted in a very scar-saving manner,
however, a higher rate of correction procedures was necessary to
individually adjust skin shrinking and thereby optimising the
prior aesthetic results.
Combined Hysterectomy/Salpingo-Oophorectomy and
Mastectomy is a Safe and Valuable Procedure for Female-to-Male
Transsexuals.
Ott, J., van Trotsenburg, M., Kaufmann, U., Schrögendorfer, K.,
Haslik, W., Huber, J. C. and Wenzl, R. (2010). Journal of Sexual
Medicine, 7: 2130–2138. doi: 10.1111/j.1743-6109.2010.01719.x
Chest-wall
contouring surgery in female-to-male transsexuals: a new
algorithm.
Monstrey S, Selvaggi G, Ceulemans P, Van Landuyt K, Bowman C,
Blondeel P, Hamdi M, De Cuypere G. Department of Plastic Surgery,
Gent University Hospital, Belgium. Plast Reconstr Surg. 2008
Mar;121(3):849-59.
Skin excess and skin elasticity are the key factors in choosing
the appropriate technique for subcutaneous mastectomy. Although
the complication rate is low and patient satisfaction is high,
secondary aesthetic corrections are often indicated.
Mastectomy for Female to Male Transsexuals.
NAMBA YUZABURO (Okayama Univ., JPN) TSUTSUI TETSUYA (Okayama
Univ., JPN) KIMATA YOSHIHIRO (Okayama Univ., JPN) KOSHIMA ISAO
(Univ. Tokyo, Graduate School of Medicine, JPN). Japanese Journal
of Plastic & Reconstructive Surgery,
VOL.49;NO.9;PAGE.985-991(2006).
Clinical experiences and information about mastectomy for FTM
transsexuals.
Breast
cancer after bilateral subcutaneous mastectomy in a
female-to-male transsexual.
Burcombe RJ, Makris A, Pittam M, Finer N. Breast. 2003
Aug;12(4):290-3.
Female-to-male transsexual, aged 33, who developed breast cancer
10 years after cosmetic bilateral subcutaneous mastectomy and
nipple reimplantation. The complex hormonal pathways involved and
the implications of undergoing prophylactic mastectomy because of
a high risk of familial breast cancer are discussed.
Circumareolar
mastectomy in female-to-male transsexuals and large
gynecomastias: a personal approach.
Colic MM. Aesthetic Plast Surg. 2000 Nov-Dec;24(6):450-4.
This technique provides naturally flat masculine breasts, leaving
sufficient dermal vascularization for the nipple-areola complex
which is of the utmost importance. All the patients were very
satisfied with the result because of the periareolar scar only.
Chest
wall contouring for female-to-male transsexuals: Amsterdam
experience.
Hage JJ, Bloem JJ. Ann Plast Surg. 1995 Jan;34(1):59-66.
At the Academic Hospital of the Free University (Amsterdam, The
Netherlands), usually one of three techniques is applied for a
subcutaneous mastectomy. We describe and discuss our experience
with 70 patients operated on before April 1993.
Back to Top Surgery Resources »
Last updated: 01/30/25