The Ultimate FTM Top Surgery FAQ
 Paying for Top Surgery
Paying for Top Surgery- Choosing a Surgeon
- Choosing a Procedure
- Eligibility & Requirements
- Preparing for Top Surgery
- Top Surgery Recovery and Post-op Care
- Other Health Considerations with Top Surgery
- Have a question? Post it here.
Paying for Top Surgery
How much does FTM Top Surgery cost?
The cost of Top Surgery
varies depending on the procedure, Surgeon and Surgeon location. See Top Surgery Costs for a range of fees for Surgeons across North America and in countries around the world.
Are there any financing options available to help me pay for Top Surgery?
To the best of our knowledge, there are no Surgeons offering private financing. Dr. Sherie and Dr. Steinwald have layaway plans. There are numerous medical finance companies that can help you pay for Top Surgery, as well as surgery grants. See Top Surgery Financing for more information.
Will insurance cover my Top Surgery?
There's no simple way to answer this question.
You'll need to take a close look at your policy. For more information about Top Surgery and insurance, see: FTM Top Surgery Insurance Coverage
Will Medicaid cover my Top Surgery?
Several U.S. states have have clarified that the state Medicaid program covers transition-related care. Even so, finding a surgeon who takes Medicaid for Top Surgery can be challenging. For more information about Top Surgery and Medicaid coverage, see: Surgeons Who Accept Medicaid For Top Surgery
Which Surgeons are accepting Medicare for Top Surgery?
You can find a list of Surgeons who are accepting Medicare for Top Surgery here. Due to low reimbursement payments from Medicare, Surgeons operating in a University/teaching or government hospital are more likely to accept Medicare than Surgeons who have a private practice. Note: Medicare only covers individuals who 1) are age 65 and older, or 2) have been on Social Security Disability Insurance (SSD or SSDI) for 2 years.
Choosing a Surgeon
Who is the best FTM Top Surgery Surgeon?
This is a common question, and the answer is... there is no "best" Surgeon for Top Surgery! "Best" is subjective--highly dependent on one's personal experience. Plus, most trans guys will only have surgery with one Surgeon—how can they compare to others? Since everyone is unique, and since Surgeons have different techniques, prices, location, etc., the question to ask isn't "who's the best Surgeon?" but "which Surgeon is best suited to my needs?"
Do I need a Surgeon who specializes in FTM Top Surgery?
Yes, this is preferable. While there are Surgeons who do a very good job on occassional Top Surgeries, there are a number of reasons for seeing a Surgeon who specializes in Top Surgery. Experience is the obvious benefit. An experienced Surgeon will produce more consistent results and knows what to do if complications arise. Also, when a Surgeon specializes in Top Surgery, the facility they use is much more likely to be trans-friendly. Be sure to ask your surgeon how many Top Surgeries they have done and how many they do per week or month. Also ask to see photos of their patients' results.
How do I choose a Surgeon to perform my Top Surgery?
Take the time to do some thorough online research. This might involve reading blogs, watching YouTube videos, and checking out before and after photos (especially from people with a similar body type to your own.) Through the process of learning about Top Surgery procedures and Surgeons, you'll develop a good sense of which Surgeon is right for you. There's much to consider: what procedures they offer, their geographic location and wait list, your budget, etc., so it's important not to rush a decision. Make a pros and cons list, assess (and re-assess) your budget, and keep your options open as you learn about the Surgeons available to you. If you make an informed and strategic decision based on your needs, you won't be disappointed with your choice of Surgeon. Find a Surgeon »
Choosing a Procedure
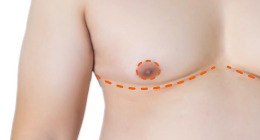
How do I know which type of Top Surgery procedure to choose?
The Surgeon that you consult with will give you their professional opinion as to the most suitable procedure based on your body type, chest size, and skin elasticity, as well as your Top Surgery goals, which might include low revision rate, low scarring, preferences for nipple and areolar size and placement, sensation etc.
Can I get a Nipple Reduction at the same time as Top Surgery?
If you're having Double Incision Top Surgery, resizing of the areola and nipple is part of the nipple graft process. With nipple-sparing Top Surgery techniques, like Keyhole and Peri-areolar, nipple size and projection may need adjustment for a more male appearance. Some surgeons perform nipple reduction during the initial surgery but it is often delayed and done as a secondary revision procedure due to blood supply.
 "It depends on how the nipple/areola looks at the end of the surgery," says Dr. Michelle Lee, a Top Surgery surgeon in Beverly Hills and star of hit TV show, Dr. 90210. "Sometimes with an aggressive peri-areola surgery, the blood supply to the nipple looks a little beat up and doing the nipple reduction might kill the nipple. I then stage the nipple reduction. If the blood supply looks good at the end of the case, I will then do the reduction at the same time."
"It depends on how the nipple/areola looks at the end of the surgery," says Dr. Michelle Lee, a Top Surgery surgeon in Beverly Hills and star of hit TV show, Dr. 90210. "Sometimes with an aggressive peri-areola surgery, the blood supply to the nipple looks a little beat up and doing the nipple reduction might kill the nipple. I then stage the nipple reduction. If the blood supply looks good at the end of the case, I will then do the reduction at the same time."
What are "dog ears" and can they be avoided?
"Dog ears" is a term that refers to excess skin and fat that "pucker" out at the primary incision line as it goes around the side of the chest in Double Incision Top Surgery. "Dog ears" are probably the most common reason for a revision surgery after Double Incision. It's a good idea to find out if dog ear repair is covered in your surgeon's revision policy as the revision surgery can cost almost as much as the original surgery. There's a growing number of surgeons who are able to consistently avoid dog ears with Double Incision by doing additional liposuction at the sides of the chest, below the arm pits. You can also help avoid dog ears by staying close to your ideal weight before FTM Top Surgery.
Eligibility & Requirements
Do I need to be on testosterone before I can get Top Surgery?
No, WPATH Standards of Care do not require hormone therapy to be eligible for Top Surgery. (An exception to this is if you are trying to get U.S. insurance coverage for Top Surgery, in which case you may find that 1 year of HRT is required by the insurance company.) One benefit of being on T prior to surgery is that it can help you develop larger chest muscles, giving your Surgeon more of a contour to work with, which can improve surgery results. However, this can also be achieved with push-ups and no testosterone.
Will I need to see a therapist to be eligible for Top Surgery?
Possibly. Many Surgeons require a letter from a mental health professional that assesses your readiness for surgery. For some guys, the process of obtaining that letter can takes months to years, depending on access, finances, and in some cases, "gatekeeping" on the part of the therapist.
On the other hand, there are also Surgeons who use the Informed Consent model, and will provide services without a therapist's letter. Find out more about Informed Consent here.
What are the WPATH Standards of Care?
The Standards of Care (SOC) for the Health of Transsexual, Transgender, and Gender
Nonconforming People is a publication of the World Professional Association for Transgender Health (WPATH). The overall goal of the SOC is to provide clinical guidance* for health professionals to
assist transsexual, transgender, and gender nonconforming people with safe and effective pathways to maximize their overall health,
psychological well-being, and self-ful?llment. This assistance may include primary care, gynecologic
and urologic care, reproductive options, voice and communication therapy, mental health services (e.g., assessment, counseling, psychotherapy), and hormonal and surgical treatments. The SOC are based
on the best available science and expert professional consensus.
The WPATH Criteria for FTM Top Surgery are:
- Persistent, well-documented gender dysphoria
- Capacity to make a fully informed decision and to consent for treatment
- Be of the age of majority in the country of surgery (and follow SOC rules for children and adolescents*)
- Significant medical or mental health concerns, if present, must be reasonably well controlled at the time of surgery
*Note: The Standards of Care are guidelines only, not rules or laws, and not all Surgeons use WPATH criteria.
I'm 16 years old. Can I get Top Surgery?
Some Surgeons require clients to be 18 years or older for surgery, while others will perform surgery on those younger than 18 with parental consent. From the WPATH SOC:
Chest surgery in FtM patients could be carried out earlier, preferably after ample time of living in the desired gender role and after one year of testosterone treatment. The intent of this suggested sequence is to give adolescents sufficient opportunity to experience and socially adjust in a more masculine gender role, before undergoing irreversible surgery. However, different approaches may be more suitable, depending on an adolescent’s specific clinical situation and goals for gender identity expression.
Preparing for Top Surgery
I'm a smoker. Will this impact my Top Surgery at all?
You will need to stop smoking at least 2 weeks before your surgery. Since you'll be tobacco-free for at least 2 weeks, why not quit altogether? Some Surgeons refuse to operate on smokers. Smoking affects anesthesia, which may increase your OR fees, and smokers usually require more oxygen after surgery. Smoking also increases the risk of failed nipple grafts and delayed wound healing. Why take on these increased risks? Make quitting smoking a priority now. (If you smoke cannabis, read this.)
What should I do to best prepare my body for surgery?
If you smoke, stop smoking. (See above.) Eat a healthy, balanced diet and exercise regularly. Increasing the muscle on your chest will provide more contour for the Surgeon to work with, improving aesthetic results. Do not drink alcohol for two weeks prior to surgery as it can increase bleeding and bruising. Your Surgeon may request that you stop taking testosterone for 2-4 weeks prior to surgery. If you are on any other medications, you should discuss them with your Surgeon, and potentially the anesthesiologist.
Do I need to stop taking testosterone prior to or immediately after surgery?
Definitely have this discussion with your Surgeon as there are different opinions about this. There are two main reasons that Surgeons recommend stopping T before and/or after surgery:
- Some studies have shown a correlation between testosterone levels and delayed wound healing
- Testosterone tends to thicken blood, increasing the risk deep vein thrombosis (blood clots.)
 Both of these reasons have been debated, and there's some evidence that suggests that testosterone actually helps with the prevention of post-operative deep vein thrombosis and eases pain from incisions. New research (2018) has revealed that there's actually little evidence to support the practice of stopping Testosterone prior to Top Surgery.
Both of these reasons have been debated, and there's some evidence that suggests that testosterone actually helps with the prevention of post-operative deep vein thrombosis and eases pain from incisions. New research (2018) has revealed that there's actually little evidence to support the practice of stopping Testosterone prior to Top Surgery.
If there's a chance of improved healing without T, then it's probably worth stopping—unless you're one of those guys who experiences a big drop in mood and energy levels without T. Either way, discuss with your Surgeon.
Also see: List of Medications to Avoid Before and After Top Surgery
Will my Surgeon cancel my surgery if I have a cold?
If you have a cold or flu with your surgery day fast approaching, it's possible that your Surgeon will want to postpone your surgery. Contact your Surgeon right away to discuss your symptoms and options.
How long does the procedure take?
Time to complete Top Surgery in the OR varies by
procedure and by Surgeon. Generally speaking, Double Incision takes about 2-4 hours, Peri-Areolar 3-4 hours, and Keyhole 1.5-3 hours.
Top Surgery Recovery and Post-op Care
Will I need to stay overnight in the hospital for Top Surgery?
Most Top Surgeries are done on an outpatient basis, either in a hospital or a private "ambulatory" clinic (facilities that offer same-day surgical care.) In other words, you'll be able to go back to where you are staying the same day as your surgery. Overnight stays would only be required if there are other health concerns that need to be monitored during the immediate recovery period, such as respiratory conditions, bad reactions to anaesthesia, and history of blood clots.
If you're travelling from out of town for Top Surgery, you'll need to stay in the area for about 7-10 days for your post-operative appointment(s) with your Surgeon. Be sure to ask your surgeon about local hotel discounts. Note that it's mandatory to have a caregiver with you during this time. Many surgeons will arrange for an overnight and/or daily check-in medical caregiver to assist you. Your caregiver can also be a friend or loved one, but they need to be comfortable with wound care and providing physical—and often intimate—assistance.
Will I need to wear a binder after my Top Surgery?
Possibly, the answer depends on the procedure that you have and your surgeon's preference. Post-operative compression plays an important role in the healing process. While wearing a binder after surgery can cause some discomfort, compression helps to minimize bruising and swelling and holds the surgical area firmly in place, supporting the intended chest contour. The binder may or may not be provided to you by your surgeon (be sure to inquire.) In general, a compression binder is worn for 3-6 weeks post-op. Follow your surgeon's recommendations regarding post-operative compression.
What is the purpose for wearing the Ace bandage after surgery?
Some surgeons recommend using an Ace bandage instead of a binder for post-operative compression. The reasoning, presumably, is that Ace bandages are cheaper than a medical-grade compression binder.
Will I have drains after my Top Surgery?
This will depend on which procedure you have and what your Surgeon recommends, but if you're having double incision or peri-areolar Top Surgery then it's likely that you will have drains. After you leave the hospital or clinic, you will need to empty your drains periodically throughout the day for up to a week. Your Surgeon or a nurse provide instruction. There are some surgeons who don't use drains. For example, Dr. Alan Dulin in Texas helped pioneer a Top Surgery method that doesn't use drains. Also see: Post-Surgical Drains: Are They Really Necessary?
Will I be in much pain after surgery?
This is highly dependent on the individual but generally the pain is less than moderate. Many Surgeons prescribe Percocet or Vicodin for post-operative pain, but for many Tramadol or Tylenol suffice.
Will I need to have any stitches taken out after my Top Surgery?
This depends on the methods of your Surgeon. Some Surgeons use absorbable subcuticular suture which is naturally absorbed and does not require removal. Other Surgeons will have you return to their offices about a week after surgery to remove non-absorbable types of sutures.
What will I need to do to take care of my chest after surgery?
You will receive post-operative instructions from your Surgeon about how to care for your incisions, and how to empty your drains (if you have them.)
How much time will I need to take off work/school after my Top Surgery?
For work, the answer depends on the type of job that you have. If you have a desk job, plan to go back 1-2 weeks later. Two weeks is recommended. If you have a more active job, that perhaps includes lifting and other more active work duties, it's recommended that you take 4-6 weeks off following surgery. Students will want to take 1-2 weeks off classes, and 4-6 weeks off of sports.
When can I go back to the gym for regular workouts?
Light activity such as walking is recommended only days out of surgery. It promotes good healing. For more strenuous workouts, with weight training especially, you should wait 6-8 weeks minimum. Bodybuilders who have had the double incision Top Surgery should take note that heavy chest workouts should be avoided for even longer, up to 3 months, to avoid stretching the incision scars.
When can I start sleeping on my side?
You will know!
When can I take a shower or bath, or soak in a hot tub?
Ask your surgeon about this. Some surgeons say you can shower after 24 hours, but you should shower with your back to the shower head to protect your healing incisions from the direct spray of the water. Afterward, gently pat the chest dry and follow any instructions your surgeon has provided regarding ointments and dressings. Other surgeons would prefer that you not shower until after your first post-operative appointment. You can bathe after surgery, but don't soak in a deep tub—keep your chest from soaking. You can use a hot tub 6-8 weeks post-operatively, but only for short periods. Do NOT use a hot tub if you have any incisions that have not completely closed. Wait 6 months to resume longer soaks.
How can I minimize the scars from my Top Surgery?
There are many things that can be done to minimize Top Surgery scars, and your Surgeon will make specific recommendations. Your incisions will likely be taped for a week or more after surgery to prevent stretching the incisions and creating wider scars. Wearing a compression vest after surgery will also help minimize scars. Silicone gel and silicone gel sheets have been proven quite effective in numerous studies, and there are many other natural products for scar healing available. Prepare your home for your return after Top Surgery by moving frequently accessed items down from higher locations, as reaching up over your head soon after surgery will stretch the incisions and the resulting scars. For example, take that favorite cereal bowl down from the 3rd shelf and put it on the counter so that you don't have to reach up to get it post-operatively. Lastly, keep your scars out of the sun, or use a strong sunscreen for a minimum of one year.
Other Health Considerations with Top Surgery
Does FTM Top Surgery eliminate the risk of breast cancer?
There's no definitive answer because there are no studies that have tracked the incidence of post-op breast cancer in trans men. The general thinking on the subject is that the risk of cancer is greatly reduced by having Top Surgery because the procedure removes almost all breast tissue. Less breast tissue = less tissue that could harbor cancer cells. However, not all breast tissue is removed, and the theory doesn't account for HRT: some trans men experience heightened estrogen levels (via aromatase) and this can increase the risk of breast cancer, even in trans men who have had Top Surgery. Other considerations include personal and family health history.
Reference: Breast Cancer and FTM Top Surgery
Will I need to continue breast cancer screening after Top Surgery?
If you are over 40 years of age your doctor should perform a breast examination using palpation of the chest and underarms at your annual check-up. If any abnormalities are found, a CT or MRI should be obtained.
Source: Breast Cancer Screening After Breast & Chest Surgery
Last updated: 12/02/2022