Sponsored Article
 Top Surgery Considerations for Non-Binary Folks
Top Surgery Considerations for Non-Binary Folks
People who identify as non-binary or genderqueer represent a substantial and growing population within the LGBTQ community. Despite this, healthcare practices have been slow to catch up to meet the needs of non-binary people seeking a medical transition/alignment.
When it comes to Top Surgery, non-binary folks often face an uphill battle accessing appropriate care. For example, securing insurance coverage can be difficult. Finding a surgeon who is not only comfortable and experienced working with non-binary patients but also knowledgeable about the surgical options for obtaining a less binary Top Surgery result can also be challenging. The good news is that there are ways around the insurance hurdles, and there are surgeons who not only have ample experience with non-binary patients but who have also put practices in place to ensure that non-binary patients feel understood and respected throughout their Top Surgery experience.
Non-binary individuals identify as neither exclusively male or female. The 2015 US Trans Survey, which included 28,000 participants, revealed that 35% of trans respondents identified as non-binary. Of those, 80% were female assigned at birth (FAAB.)[1] A more recent study shed more light on the number of people who identify as one of the many terms that fall under the non-binary umbrella:
In a 2017 survey published by the LGBTQ media advocacy group GLAAD, 12 percent of respondents between 18 and 34 identified with a gender identity other than the one they were assigned at birth. Three percent of those surveyed identified as "agender"; 3 percent as "gender fluid"; 2 percent as "transgender"; 2 percent as "unsure/questioning"; 1 percent as "bigender"; and 1 percent as "genderqueer." [2]
Non-binary individuals may want hormones and surgery, hormones but not surgery, surgery but not hormones, or neither hormones or surgery. In one study, 77.2% of non-binary participants indicated that they had some interest in using hormones or surgery to alleviate gender dysphoria, while 17.7% expressed no interest, and 6.3% indicated that they had already completed all medical transition interventions that they would like.[3]
In a healthcare setting, non-binary people often feel misunderstood and face pressure by healthcare providers to "transition fully"[4], to conform to binary medical narratives[5], or to transition according to a standard formula:
"The standard formula is you get on hormone replacement, and then you get top surgery, and then you get bottom surgery. You would handle all that in those steps. And that's the standard idea in the medical field. And you know that narrative doesn't apply for every binary trans person. It's even less clear sometimes what people need if you're non-binary." - Non-binary patient in the UK [6]
The WPATH Standards of Care requirements for having Top Surgery are pretty straightforward:
- Persistent, well-documented gender dysphoria;
- Capacity to make a fully informed decision and to consent for treatment;
- Age of majority in a given country (if younger, follow the SOC for children and adolescents);
- If significant medical or mental health concerns are present, they must be reasonably well controlled.
Hormone therapy is not a pre-requisite. [7]
Despite guidelines to the contrary, transgender people are routinely required to take Testosterone for a year before they can have Top Surgery. Requirements put into place by medical professionals to control who gets access to medical transition is called gatekeeping.
"I needed top surgery before I knew whether or not hormones were right for me," says CJ. "That was too much for the clinic. They are very clear they want you to go down a certain route. I was told by my doctor that I'd have to go to counseling until I decided to take hormones first, because I couldn't know what I wanted otherwise. But that's nonsense because I'd been binding my chest (painfully and dangerously) for a few years, and at the time my chest was my only source of discomfort. - CJ, non-binary patient in the UK [8]
Getting Insurance To Cover Non-Binary Top Surgery
Non-binary people who are paying for Top Surgery out-of-pocket can move forward with a surgeon who uses the informed consent model—a letter of medical necessity isn't required. If the surgeon doesn't use informed consent, then a letter of medical necessity from a qualified mental health professional is required.
Non-binary folks who want to use insurance for Top Surgery may face more hurdles. Insurance plans that include transgender benefits often require the patient to identify as a binary gender. In this case, the therapist writing the required letter of medical necessity should understand how to write the letter to satisfy insurance requirements, for example using he/him pronouns. In cases where a binary identity is not required, the letter should document specifically how long one has lived as non-binary and used their current name. Typically, insurance companies want trans patients to follow the standard transition formula that focuses on certain treatments carried out in a specific order, essentially nullifying the existence of those who don't subscribe to that standard. The truth however is that in some cases and with certain insurance companies, you don't need to be on hormones or live as a particular gender to receive coverage for Top Surgery.
The Guide for Insurance Coverage for Top Surgery In the United States walks you through the process of getting insurance coverage for Top Surgery and it's important to note that it was authored by a non-binary individual who is not on Testosterone, lives in state that had no legal protections at the time, and had an insurance plan with exclusions—yet they still got their Top Surgery covered! In clear language, this step-by-step guide will help you understand how to:
- Determine if your insurance plan covers Top Surgery
- Meet the criteria for medical necessity
- Find a surgeon who is in-network with your health insurance
- Get a surgery consultation
- Submit a request for pre-authorization
- File an appeal if you are denied coverage (appeal letter template included.)

Dr. Scott W. Mosser, MD, FACS
is a board certified, award-winning plastic surgeon who is an expert at performing several types of gender affirming Top Surgery and Body Contouring procedures. Based in San Francisco, Dr. Mosser sees patients from around the country.
Finding a Surgeon With Non-Binary Experience
When seeking Top Surgery as a non-binary person, finding a surgeon with the right experience is an advantage that's hard to put a price tag on. Surgeons who regularly work with non-binary patients have processes in place to help ensure that their practice offers a gender affirming environment for all patients. Examples of this are inclusive healthcare forms that have non-binary gender and pronoun options, and fields for legal and currently used names; and gender affirming written and verbal communications from the surgeon and their staff.
Dr. Scott Mosser is a surgeon in San Francisco who specializes in gender affirming Top Surgery and Body Contouring procedures. As of 2018, he has completed more than 1,000 Top Surgeries, and due to his gender affirming healthcare model many of his patients are non-binary. When Dr. Mosser noticed that his Electronic Medical Records (EMR) system was not set up for his transgender and non-binary patients he demanded changes to make the system more inclusive. Dr. Mosser was able to achieve the following changes in his EMR systems [9]:
- Distinction between assigned sex (male, female, intersex) and gender identity (male, female, neutral/non-binary)
- Distinction between legal name and name the patient uses
- Pronouns (he/him, she/her, they/them, ze/hir)
Non-Binary Top Surgery Techniques
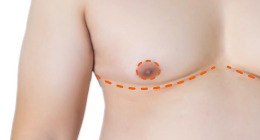
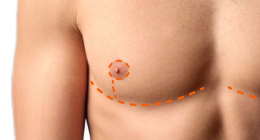
Having worked extensively with non-binary patients, Dr. Mosser is well-versed in the techniques that can achieve the outcomes that non-binary patients often desire. Different approaches to incision location and shape, and chest contours, plus a number of nipple and areola options are available for those seeking a less binary and more customized Top Surgery result.
In non-binary Top Surgery:
- Incisions can be longer, higher or lower, or more straight than the typical binary approach to Top Surgery;
- Chest contours can be less masculine, with more chest tissue left behind;
Tip from Dr. Mosser: In cases where a patient has a particular wish regarding the exact amount of chest tissue to be left over, I highly advise them to bring in photos of bodies that have the amount of chest tissue that they would be hoping to have at the conclusion of surgery. This helps to avoid any misunderstandings regarding what the procedures can offer and what the limitations of each procedure type are for a given body type are. - Areola size can be made more narrow or larger than what is typically done in Top Surgery;
- Nipples can be left with more projection;
- Location of the nipple-areola complex (NAC) can be higher.
Tip from Dr. Mosser: When patients choose a wider areola, a slightly higher placement seems to be overall aesthetically most pleasing. - Nipples can be omitted completely (in a Double Incision procedure.)
"Scar shape is a discussion that I love to have with patients because it brings art and creativity into our discussion. It is my opinion that there are not specifically masculine scars, nor are there scars that are only 'meant for' nonbinary patients. There are different types of scars that some patients may be more drawn to, which may or may not be related to gender identity." — Dr. Laurel Chandler
Non-binary folks interested in having Top Surgery may face some hurdles getting to the finish line, but should also know that there are ways around insurance as well as experienced surgeons like Dr. Mosser who are enthusiastic about providing truly inclusive care.
References:
1. US Trans Survey, http://www.ustranssurvey.org/reports
2. Tatyana Bellamy-Walker, "For nonbinary patients, seeking health care can be a painful task", nbcnews.com
3. Hannah Mogul-Adlin. "Unanticipated: Healthcare Experiences Of Gender Nonbinary Patients and Suggestions For Inclusive Care." January 2015. https://www.mobt3ath.com/uplode/book/book-8601.pdf
4. Hannah Mogul-Adlin.
5. James E. Lykens, MA, Allen J. LeBlanc, PhD, and Walter O. Bockting, PhD, "Healthcare Experiences Among Young Adults Who Identify as Genderqueer or Nonbinary." LGBT Health, Volume 5, Number 3, 2018 https://www.ncbi.nlm.nih.gov/pubmed/29641314 | [FULL PDF]
6. Lykens et al.
7. WPATH Standards of Care
8. Chris Godfrey, "How the Healthcare System Screws Over Non-Binary People", Mar 14 2016, broadly.vice.com
9. "Non-Binary Standards of Care", genderconfirmation.com
Related Journal Articles
A Comparison of Gender-Affirming Chest Surgery in Nonbinary Versus Transmasculine Patients.
McTernan M, Yokoo K, Tong W. Ann Plast Surg. 2020 Feb 6.
Increasingly more nonbinary patients are obtaining better access for gender-affirming chest surgery (top surgery), representing an important subset of patients who undergo such surgery.
There were 111 nonbinary patients and 665 transmasculine patients included in the final analyses.
What is "Nonbinary" and What Do I Need to Know? A Primer for Surgeons Providing Chest Surgery for Transgender Patients.
Esmonde N, Heston A, Jedrzejewski B, Ramly E, Annen A, Guerriero J, Hansen J, Berli J. Aesthet Surg J. 2019 Apr 8;39(5):NP106-NP112.
This was an observational study of nonbinary patients who underwent "chest-affirming surgery" from 2012 to 2017.
A total of 458 patients with gender dysphoria underwent chest surgery; 58 (13%) patients were nonbinary. The most commonly performed procedure was the double incision technique with nipple grafts (72%). Chest surgery for nonbinary patients comprises a considerable proportion of transgender surgery practice, and surgeons who provide affirming care should be familiar with the unique characteristics and treatment options for this population.
Last updated: 11/14/22