Sponsored Article
Demystifying Liposuction & Body Sculpting
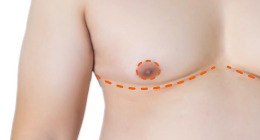
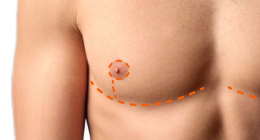
What You Need to Know If You're Considering Body Masculinization Surgery
 In the context of gender-affirming surgery, Body Sculpting procedures are commonly referred to as Body Masculinization Surgery (BMS). While BMS is growing in popularity, it's not new: BMS uses well-established Liposuction techniques to offer a surgical solution for altering body shape when diet, exercise and Testosterone therapy fall short.
In the context of gender-affirming surgery, Body Sculpting procedures are commonly referred to as Body Masculinization Surgery (BMS). While BMS is growing in popularity, it's not new: BMS uses well-established Liposuction techniques to offer a surgical solution for altering body shape when diet, exercise and Testosterone therapy fall short.
When researching Liposuction online, you'll find a confusing soup of different names for different types of Liposuction. Additionally, a number of new Liposuction technologies have been marketed to surgeons and their patients. This amounts to a growing need for clear information about each method and their effectiveness for Body Masculinization.
What Is Liposuction?
Liposuction is a method of removing fat cells using suction and damaging the remaining fat cells, which are absorbed by the body over 2-3 months after surgery.
When Liposuction was initially developed in the late seventies, it was performed without the introduction of fluid (Dry Liposuction). Later, a small amount of fluid was injected into the fat (Wet Technique). In 1985, Tumescent Liposuction was introduced as a method that used a specific fluid to make the fat easier to target, and also reduced blood loss. Strictly speaking, the term "Tumescent Liposuction" refers to a technique that does not use general anesthesia, but in practice local or general anesthesia may be used, with the term referring more generally to the use of Tumescent fluid. However "Tumescent" is also commonly dropped, leaving simply "Liposuction" as the term that describes Liposuction with the use of Tumescent fluid, the worldwide standard of care for Liposuction.

SOURCE: Tumescent Liposuction: A Review by Jayashree Venkataram. J Cutan Aesthet Surg. 2008 Jul-Dec; 1(2): 49–57.
Suction-Assisted vs. Power-Assisted Liposuction?
Suction-Assisted Liposuction (SAL), also called Manual Liposuction, is the traditional Tumescent technique first introduced in 1985. It requires the surgeon to push and pull the Liposuction cannula through the fatty tissue to be removed, requiring physical effort and precision. Power-assisted Liposuction (PAL), introduced in 1998, uses a powered cannula that vibrates rapidly while being moved through the fatty tissue, reducing physical exertion and shortening operating time. Proponents of PAL claim that it causes less tissue trauma resulting in less post-operative swelling and discomfort. However, in a study published in 2011, neither SAL or PAL demonstrated a distinct advantage over the other in the post-operative evaluations for bruising, swelling, results, recovery times and complications. Both techniques use Tumescent fluid. What's important is not whether the Liposuction cannula your surgeon uses is powered or not, but their experience and success using the technique they offer.
 Dr. Scott W. Mosser is a Board Certified Plastic Surgeon who is an expert at performing all types of FTM/N Top Surgery, as well as Body Sculpting Liposuction. He is often able to perform Body Masculinization at the same time as Top Surgery. Dr. Mosser generally uses Suction-Assisted Liposuction but sometimes uses Power-Assisted Liposuction.
Dr. Scott W. Mosser is a Board Certified Plastic Surgeon who is an expert at performing all types of FTM/N Top Surgery, as well as Body Sculpting Liposuction. He is often able to perform Body Masculinization at the same time as Top Surgery. Dr. Mosser generally uses Suction-Assisted Liposuction but sometimes uses Power-Assisted Liposuction.
Innovation or Just Good Marketing?
In recent years, a number of new Liposuction technologies have been marketed and you're likely to come across these in your search for information about Body Masculinization:
- Ultrasound-Assisted Liposuction (Internal – UAL; External – XUAL; also includes VASER Hi-Definition Liposuction™): Uses an internal or external method to administer ultrasound that emulsifies fat before suction. Claims to be more selective in the destruction of fatty tissue, more effective for fat removal while minimizing trauma to surrounding tissues, and reduce the risk of lumpy/dimpled results.
- Laser Liposuction (Coollipo™, Smartlipo™, Slimlipo™): Uses laser to emulsify fat before suction. Claims to be more selective in the destruction of fatty tissue, reduce bruising, and tighten skin.
Dr. Mosser has tried many different types of Liposuction throughout his career as a Plastic Surgeon, and has not found any of them to be game-changers for his patients. He also feels that many of them have been marketed in a deceptive manner:
"Some of the laser-assisted liposuction technologies are marketed to have no downtime and no pain during the procedure when done under local anesthesia. I can definitively say that this is not the case. Generally, I perform liposuction under general anesthesia because I want the patient to be perfectly comfortable and I want to be able to get to the best aesthetic endpoint that I can achieve without having to shortchange a result because an environment cannot achieve full comfort for a patient." — Dr. Scott Mosser
Legally, any doctor can perform Liposuction, and CoolSculpting™ can be done by any technician certified to use the CoolSculpting™ machine. (CoolSculpting™ is a non-surgical fat reduction technique that does not use Liposuction at all. Fat cells are killed by freezing and absorbed by the body.)
With so many Liposuction options, what's the best way to proceed for those interested in Body Masculinization? Dr. Mosser's advice is to work with a Board-Certified Plastic Surgeon who has meticulous attention to detail with a tried-and-true approach.
If you're interested in Top Surgery with Body Sculpting, or if you have questions about which Liposuction methods would be most effective for Body Masculinization, ask Dr. Mosser here.
Further Reading: A journey through liposuction and liposculpture: Review
Elisa Bellini, Michele P. Grieco, and Edoardo Raposio. Ann Med Surg (Lond). 2017 Dec; 24: 53–60.
Last updated: 08/17/23